US FDA Issues Technical Guidance for Medical Devices using 3-D Printing
有任何问题?向我们的专家获取相关信息
联系我们2016年 5月 16日
New draft guidance from the US Food and Drug Administration covers premarket and quality system issues concerning medical devices incorporating additive manufacturing (AM), or 3-D, printing and fabrication techniques.
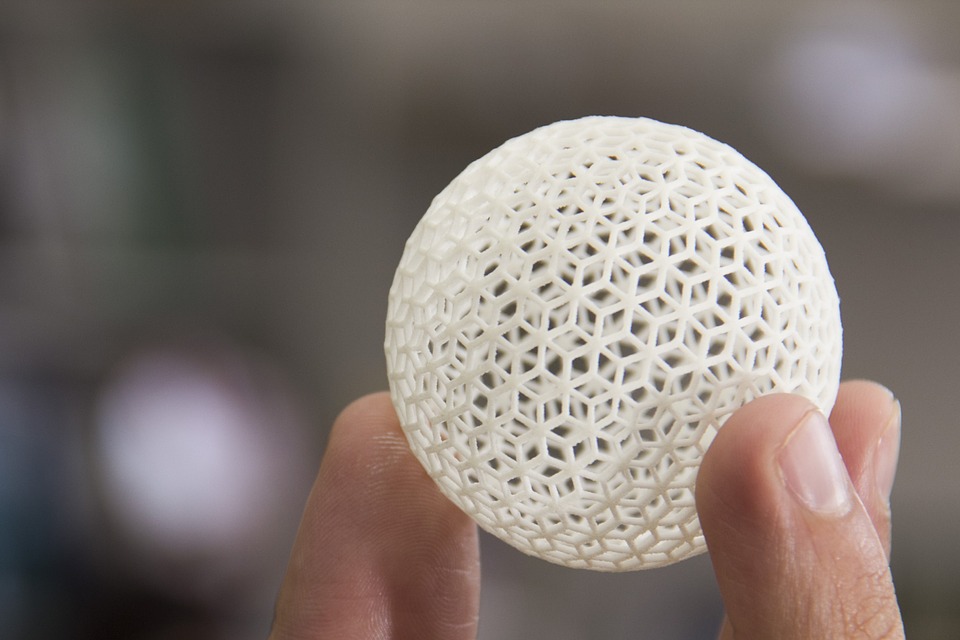 Additive manufacturing has major implications for medical device design in terms faster and more efficient design changes without having to undertake expensive and lengthy retooling.
Additive manufacturing has major implications for medical device design in terms faster and more efficient design changes without having to undertake expensive and lengthy retooling.
The FDA guidance encompasses technical “design and manufacturing considerations” and “device testing considerations,” which deal respectively with quality system compliance and premarket review submissions. The agency refers to the new guidance as“leap-frog” guidance, meaning that the document represents initial FDA considerations and recommendations related to emerging technologies such as additive manufacturing.
It is important to note that the new guidance focuses only on design, manufacturing and testing issues related to devices with 3-D components—the FDA has stated that the new publication does not indicate a comprehensive regulatory approach to such devices. As 3-D devices and technologies proliferate, US regulators will no doubt develop more in-depth guidances and requirements covering more aspects of registration and compliance.
Design and manufacturing issues
First, the FDA covers technical design and manufacturing issues devices utilizing 3-D printing or fabrication should address in order to meet general quality system requirements. Design recommendations, according to the guidance, depend on several factors:
- Device design: AM devices offered in discrete sizes based on standard-sized designs versus patient-matched device designs based on standard templates but then customized or scaled to individual patients’ anatomies.
- Software workflows: 3-D components of AM devices require interaction between multiple software packages that may or may not work well together out of the box. Manufacturers should address issues such as file conversion errors and digital-to-physical processes for turning AM designs into actual devices.
- Material controls: Manufacturers should document any and all physical or chemical changes made to starting materials used in their AM processes, as well as all material suppliers and sources, specifications and certificates of analysis. Any recycling of materials in a manufacturer’s AM process should be documented, also.
- Post-processing: Manufacturing steps taken after final AM printing may affect final device performance; the guidance suggests thorough documentation of steps such as cleaning, final machining or annealing, as well as their effects on materials as well as on the final device.
- Process validation and acceptance: Process validation is necessary to ensure consistent quality across AM devices produced in a single build cycle, as well as between build cycles and between different machines. All monitoring methods and data generated from validation processes should be documented.
- Quality data: AM manufacturers should determine whether data such as where their devices are built should be tracked. Quality data should be available for analysis for purposes of identifying quality problems and investigating nonconformities.
Device testing
The FDA guidance also contains recommendations for types of device testing and related information AM device manufacturers should include in premarket applications such as 510(k) premarket applications and premarket approvals (PMA).
In general, according to the guidance, any performance testing that would be required for more conventionally manufactured devices would also be necessary for AM devices. Testing and other data that AM device manufacturers should include in their FDA market applications include:
- Device description: AM devices do not necessarily have discrete sizes and shapes the way conventionally manufactured devices do, so applicants should take care to describe any design variations, critical dimensions and types of 3-D technology utilized in their premarket submissions.
- Mechanical testing: This type of testing is generally the same for AM and conventionally manufactured devices; material property and performance testing typically fall under this category, and should be included in premarket submissions. Data specific to AM devices to be included in submissions include orientation and build location information.
- Dimensional measurements: For AM devices, issues of orientation and location within build spaces can affect device dimensions, so information on such issues should be disclosed to FDA reviewers. Applicants should specify dimensional tolerances and conduct dimensional measurements for all AM components of their devices, the guidance recommends.
- Material characterization: All materials used to manufacture an AM device should be identified in a premarket submission. Applicants should identify and describe material chemistry physical properties in their submissions as well.
- Cleaning and sterilization: Given AM devices’ more complex dimensions and shapes, cleaning and sterilization processes for these devices can prove challenging. Premarket submissions for such devices should include descriptions of cleaning and sterilization processes used for 3-D devices, and also justify why processes used are appropriate to properly clean and sterilize such devices.
- Biocompatibility: All finished AM devices should be evaluated for biocompatibility requirements according to the ISO 10993 standard’s evaluation and testing recommendations, and the results of such evaluations should be included in FDA applications.
- Labeling: Labeling requirements in general for AM devices are the same as for conventional devices. For patient-matched 3-D devices, however, manufacturers should add additional information such as patient identification, details of use such as anatomical location and final design iteration information to labeling.